Introduction
Our knowledge has evolved over thousands of years since man first learned
to start fires. It has evolved in a slow methodical fashion. I have been fascinated how
knowledge developed in many fields ultimately comes together synergistically to make the
whole result greater then the parts.
I will examine a narrow segment of this evolution of knowledge and talk
about how it has affected me as a consumer of today's healthcare approaches for insulin
dependent diabetes.
A Consumers Point Of View
What ultimately became the major focus of my consumer needs came to me
suddenly in 1971. I was 32. I began to experience extreme fatigue. My days at work seemed
extremely long, and I had to run to the restroom almost continuously. My wife became
concerned and tried to get me to see the doctor. As usual I told her that I would be fine.
I reminded her that I just had a bad case of the Hong Kong Flu and had probably not
completely recovered. After about two weeks I suddenly realized that I had lost about 15
pounds even though I was eating everything in sight. One Sunday I had a large dinner and
decided I was still hungry. I then ate an entire box of Sugar Pops. My wife mentioned
diabetes and again urged me to see the doctor. I said that that wasn't possible because no
one in my family had ever been a diabetic.
Finally I felt so horrible that a doctor's appointment seemed like a
wonderful idea. To the doctor my symptoms were very clear. To confirm his diagnosis he
took a blood test and after several hours of waiting for the results I was admitted to the
hospital with a diagnosis of diabetes mellitus.
I knew a little about diabetes because a family friend was diabetic. I
remembered that he boiled and sharpened his insulin needles. I also remembered that he was
supposed to be careful about what he ate. He wasn't. Obviously I had a few things to
learn.
We talked to the doctor and the dietician. We learned that diabetes was
different from most diseases in that you had to manage it. There was no cure. I would have
to consciously manage my blood sugar to keep it within a normal range. It also meant that
I would have to take daily injections forever and eat a planned diet. That wasn't very
attractive but my choices were a little limited. I had a wife and three children and I was
determined to live a normal life.
The doctor set my insulin level and the calories for my diet. The hospital
dietician prescribed a diet that was known as an exchange diet. It was a high protein diet
with limited carbohydrates. My diet and exercise would have to be predictable. I would eat
6 times a day on schedule to match the progression of the insulin.
I was also to check my urine with a litmus paper called Tes-tape. It
indicated the level of glucose in my urine. If it turned various colors it would indicate
a high blood sugar. I was to keep a record of these tests and bring it to my doctor's
office. With this knowledge I left the hospital.
After I was released I followed the regimen prescribed by the doctor and
dietician. I visited the doctor regularly to have a fasting blood glucose test and review
my Tes-tape records. Based on the results minor adjustments to my insulin or diet were
periodically made to maintain control.
Such was the state of diabetes management in 1971. How did we get there?
Where are we today?
What is Diabetes?
Let me take a moment to define Diabetes Mellitus.
The National Institute of Diabetes and Digestive and Kidney Diseases
defines diabetes as a disorder of metabolism -- the way our bodies use digested food for
growth and energy. The digestive juices break down most of the food we eat into a simple
sugar called glucose. Glucose is the main source of fuel for the body.
After digestion, the glucose passes into our bloodstream where it is
available for body cells to use for growth and energy. For the glucose to get into the
cells, insulin must be present. Insulin is a hormone produced by the pancreas, a large
gland behind the stomach.
When we eat, the pancreas automatically produces the right amount of
insulin to move the glucose from our blood into our cells. Insulin is released when we
eat. It is released in sufficient amounts to maintain blood sugar levels at the normal
range.
In people with diabetes, the pancreas produces little or no insulin, or
the body cells do not respond to the insulin that is produced. As a result, glucose builds
up in the blood, overflows into the urine, and passes out of
the body. Thus, the body loses its main source of fuel even though the blood contains
large amounts of glucose.
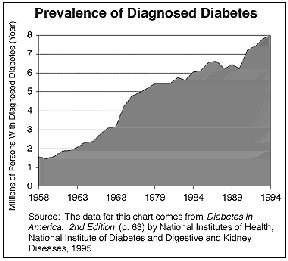
The prevalence of diagnosed diabetes has been increasing dramatically over
the past 40 years. Currently over 8 million persons have diagnosed diabetes. Approximately
5% require insulin injections to live. The other 95% use oral medication and life style
changes for control.
The Early History
I didn't know it at the time; but I was very lucky. Only 50 years before
had enough knowledge been developed to allow me to live. Before 1922 I would have died
within a very short time. To appreciate these changes we need to look back in history.
Imagine, as we look at how knowledge has evolved that you are a hard
working young man. Suddenly you are urinating far more frequently than you ever have
before. You are constantly hungry and eat everything you can. You friends tell you that
you are getting thin. You are constantly tired.
In prehistoric times your illness would most likely have been considered
the work of malevolent demons. Some medical knowledge did exist. Usually medical therapy
mounted directly against a disability was the most successful. Medical procedures
practiced in ancient societies included cleaning and treating wounds by cautery,
poultices, and sutures. Physicians reset dislocations and fractures, and used splints.
Additional therapy included the use of purges, diuretics, laxatives, emetics, and enemas.
Perhaps the greatest success was achieved by the use of plant extracts. So successful were
these that 50 or more continue to be used today. Digitalis a heart stimulant extracted
from foxglove, is perhaps the best known.
Since your illness was not a visible wound or minor ailment your primary
treatment would probably have consisted of incantations, dancing, magic effects, charms
and talismans, and various other measures. You would have died in short order.
Approximately 3500 years ago in Egypt physicians emerged as an early form
of scientist, distinct from the sorcerer and priest. The physician normally spent years of
arduous training at temple schools in the arts of interrogation, inspection, and
palpation.
In these days the physician would ask you questions examine your overall
condition and perhaps offer you some roots or other medications. Most but not all patients
died in relatively short periods of time.
The earliest written evidence of diabetes was an early Egyptian medical
text written around 1550 BC, called the Ebers Papyrus. It describes a condition of "passing too much urine." The Greek physician Aretaeus, who lived in the second
century A.D., gave diabetes its name, from a Greek word meaning "siphon" or
"pass through." Aretaeus observed that his patients' bodies appeared to
"melt down" into urine. It was again noted in the writings of the Hindu
physician Sussruta in the 4th century AD.
By the 3rd century BC, Egypt, the seat of a famous medical school and
library, was firmly established as the center of Greek medical science. In Alexandria the
anatomist Herophilus performed the first recorded public dissection. Important work on the
anatomy of the brain, nerves, veins, and arteries was carried out.
In the 7th century the Arabists elevated professional standards by
insisting on examinations for physicians before licensure. They excelled in the fields of
ophthalmology and public hygiene, introduced numerous therapeutic chemical substances, and
were superior to the physicians of medieval Europe.
Early medieval Europe suffered from complete disorganization of the lay
medical fraternity. To provide medical care, a form of ecclesiastical medicine arose;
originating in the monastic infirmary, it spread rapidly to separate charitable
institutions designed to care for the many sufferers of leprosy and other disorders. The
Benedictines were especially active in this work, collecting and studying ancient medical
texts in their library at Monte Cassino Italy. St. Benedict of Nursia, the founder of the
order, obligated its members to study the sciences, especially medicine. The abbot of
Monte Cassino was himself a famous physician.
By the end of the 12th century the revival of lay medicine and
restrictions on activities outside the cloister brought about the decline of monastic
medicine, but it had performed a valuable function by preserving the traditions of medical
learning. In the 13th century, dissection of the human body was permitted, medical
licensure by examination was endorsed, and strict measures were instituted for the control
of public hygiene, but scholastic medicine remained largely a logical exposition of
ancient dogma.
The English philosopher Roger Bacon was the first scholar to suggest that
medicine should rely on remedies provided by chemistry.
In the 17th century Thomas Willis having investigated the anatomy of the
brain and the nervous system, was the first to distinguish Diabetes Mellitus. After the
discoveries of Copernicus, Galileo, and Newton, 18th-century medicine began to adapt to
the formal scientific disciplines we know today.
Early observers noted that urine from people with diabetes was very sweet.
In fact, one test to diagnose diabetes was to pour urine near an anthill. If the ants were
attracted to the urine, it meant that the urine contained sugar. By the eighteenth
century, physicians added the Latin term mellitus, which describes the sugary taste of
diabetes.
It wasn't until 1776 that scientists discovered that glucose was in the
blood of both people with diabetes and people who didn't have diabetes. That led them to
suspect that people with diabetes pass sugar from the blood to the urine. But they didn't
know why or how.
In 1889, more than 100 years after glucose was found in blood, two German
physiologists, Oskar Minkowski and Joseph Von Meting found by accident that the pancreas
was involved in diabetes. They were investigating how fat is metabolized in the body. They
decided to remove the pancreas from a laboratory dog. Much to their astonishment, the dog
urinated again and again. Fortunately, they had previously tested the dog's urine for
glucose because the dog developed diabetes when its pancreas was removed.
This led the scientists to suspect that some substance in the pancreas
somehow prevented diabetes. Scientists embarked on a 30 year quest to find that magic
substance. Physicians treated their patients with a host of so called cures, including
bloodletting, opium, and special diets. Unfortunately, none of these measures helped the
disease. Although some diets seemed to help some older people with diabetes, they did
nothing for severely affected young patients.
Scientists and physicians had developed much basic knowledge. However over
a period of 3300 years little had changed for the patient.
TWENTIETH CENTURY PROGRESS
In 1921, Dr. Frederick Banting, a young surgeon just out of medical
school, had a breakthrough. He isolated the groups of cells called the Islets of
Langerhans in the pancreas. Working in the laboratory of a senior faculty member at the
University of Toronto, Professor J.J.R. Macleod, an authority on carbohydrate metabolism,
Banting began his experiments. Macleod teamed Banting with a young medical student named
Charles Best.
The biggest breakthrough came in 1922 when Frederick Banting and Charles
Best conducted a series of experiments.
Using laboratory dogs Banting tied off the pancreatic duct, which connects
the pancreas to the intestine. This would destroy most of the tissue of the pancreas,
which would no longer be able to secrete its digestive enzymes into the intestine. Banting
guessed that the islets of Langerhans secrete something directly into the blood and that
these cells would survive. At long last, they succeeded in treating a dog with diabetes
using extract from the islet cells. They painstakingly took fluid from healthy dogs'
Islets of Langerhans, injected it into the diabetic dogs and restored them to normalcy for
as long as they had the extract.
Within 6 months after their success the two scientists injected their
extract into Leonard Thompson, a 14-year-old boy who was dying from diabetes, but the boy
remained ill. A biochemist working in Macleod's laboratory, J.B. Collip, purified the
extract, and the experiment was re-peated 12 days later. This time the scientists
succeeded, and the boy, emaciated from diabetes, began to gain weight. He lived for 15
years with regular insulin injections, until he died from pneumonia in 1928.
Banting and Macleod were awarded the Nobel Prize in Medicine for their
discovery. Feeling that their collaborators had been slighted, Banting shared his prize
money with Best, and Macleod shared with Collip. The team had made an important discovery
leading to a diabetes treatment that is still in use today.
The University of Toronto immediately gave pharmaceutical companies'
license to produce insulin free of royalties. In early 1923, about one year after the
first test injection, insulin became widely available, and began to save countless lives.
Now for the first time in history the physician could actually give patients the hope of
living. The patient had to take insulin injections daily and was told to live a very
predictable life. Each day the patient would take the same insulin injections, the same
amount of food and the same amount of exercise. But you could live. There were side
effects. You could get hot and shaky or you could get queasy and tired. These are signs of
glucose levels that are either too high or too low. Once you made the appropriate
corrections you would feel fine.
Diabetes still could not be cured but it could be managed. The patient had
to be intimately involved in managing his own metabolism. Scientists learned that initial
insulin levels could be based on body weight and subsequent adjustments made from the
blood glucose tests. Predictability was essential.
Insulin therapy while generally successful was difficult. The patient had
to manage their life in a strict predictable manner to avoid poorly understood variations.
Very few people are capable of such absolute predictability. Much work remained.
The relationship between insulin, food and exercise had to be refined in sufficient
clarity to allow patients to manage their own health.
For safety, the patient had to be very aware of their feelings to
determine if their glucose was high or low. If your blood glucose is too high you will
pass into a coma. If your blood glucose is too low you will lose consciousness. Such
awareness is less than reliable and does deteriorate over time. This is particularly true
with hypoglycemia or low blood sugar. Diabetics did their best to follow a fixed plan in a
highly variable world. Almost anything (slow restaurants, a cold, too much exercise,
unanticipated overtime, a hidden infection, or a holiday celebration) could cause
deviation from the tight control level the physician devised.
The only way to determine blood glucose was with a lab test conducted in
the doctor's office. Results were not available in time to take any appropriate action.
The tests confirmed that the patient was in or out of control at the time of the test.
New issues evolved. Poorly controlled diabetics suffer complications of
diabetes. These include blindness, cardiovascular disease, kidney disease, ketoacidosos
and neuropathy.
Obviously more progress was still needed. Since 1922 changes have rapidly
evolved. The changes are still dramatic in their effect.
Balance and Control
Since the discovery of insulin, diabetics have been told that there are
three primary parts to the balancing their life to live with diabetes. They are insulin,
diet, and exercise. For the diabetic to live long and healthy in a perfect world:
You inject exactly the amount of insulin you need to use the glucose
generated by the food you plan to eat. This occurs several times a day. The number of
times varies depending on the regimen your healthcare team has worked out with you.
You eat exactly what you need to provide energy for your activities,
maintain a healthy weight, and provide the vitamins and minerals to keep healthy.
You exercise just enough to use exactly the energy provided by the glucose
converted by the insulin.
That's simple. Isn't it? Well not exactly. Something is still missing.
Insulin

Lets start with the insulin. Insulin enables the body to process food into
energy. Natural insulin acts rapidly. A properly functioning pancreas releases insulin on
a continuing level just to maintain body functions. When we eat it releases the exact
amount necessary to convert glucose to our cells for future use.
Initially manufactured insulin was derived from either beef or pork. It
had many impurities and an inconsistent strength. Early insulin dependent patients could
follow the prescribed regimen exactly and still experience difficulty because the insulin
had significant variability.
Technology has refined insulin to a reproducible product that is similar
to human insulin. Manufactured insulin is usually injected several times a day. The
release rate is fixed into the insulin. Typically injected insulin lasts in the body for
24 to 36 hours. A risk of hypoglycemia or low blood sugar occurs 6 to 12 hours after
injection. To accommodate variable life styles pharmaceutical companies developed short
acting, intermediate acting, and long acting insulin. . A 6:00 AM injection means that you
must eat lunch and dinner on time before lows are likely to occur.
Manufactured insulin is relatively slow. Natural insulin acts immediately
and is secreted continuously. Ideally injected insulin would mimic the body's secretion
and response. Scientists have attempted to provide this imitation by combining insulins of
different reaction times.
In 1978 insulin became the first human protein to be manufactured through
biotechnology. The result was human insulin, without the problems animal insulin sometimes
causes. Today, almost all diabetics use recombinant human insulin instead of animal
insulin.
Until recently, manufactured insulin has fallen into three categories that
describe their duration in the body. In 1996 the Food and Drug Administration approved a
modified human insulin called Lispro (brand name Humalog) which was specially developed to
be active very quickly after injection.
Types of Insulin Available
Insulin type |
Onset |
Peak |
End |
Lows most likely at |
| Natural |
Immediate |
0.5 to 1 h |
N/A |
N/A |
| Lispro |
0.25 h |
.1 to 1 1/2 h |
4 h |
1 1/2 to 4 h |
| Regular |
0.5 to 1 h |
2 to 3 h |
8 h |
3 to 7 h |
| NPH Lente |
2 to 4 h
3 to 4 h |
4 to 10 h
6 to 12 h |
22 h
24 h |
6 to 13 h
7 to 14 h |
| Ultra-Lente |
6 to 10 h |
10 to 18 h |
36 h |
10 to 22 h |
The slow release Lente or Ultra-Lente mimics the constant
secretion of insulin to allow a continuous conversion of glucose to support the body's
normal basic functions. This is the basal rate for insulin. The fast acting lispro
injected just before a meal mimics the release of insulin by the pancreas when food is
taken.

Eli Little and Company, 1996, 1999
These evolving approaches using injected insulin have effectively allowed
diabetics to live significantly longer lives. However, exact replication of the body's
actions is still not perfect and many diabetics experience complications that result from
inadequate control of their glucose level.
Diet
To live a reasonably normal life the diabetic has to balance dietary
intake with insulin and exercise.
Medical science has learned that carbohydrates primarily provide the
glucose available for conversion. Initially, after the discovery of insulin, dietary
carbohydrates were kept at a minimum because they caused the largest impact on glucose
levels. Today dieticians advise patients to eat a healthy diet that includes a balance of
all healthy foods. The diabetic needs to estimate and manage their carbohydrate intake.
But, who can realistically calculate the carbohydrates they eat? Food lists are available
in paperback books that give food content. However, it still takes a good eyeball and much
experience to know what you can reasonably eat. Care to guess how many carbohydrates are
in that Burrito Grande at Cuca's?
To put this in perspective one piece of bread can raise my blood sugar 50
points if I don't anticipate that bread with the right dose of insulin. If I catch a cold
the effect might be an increase of 100 points. The normal range of glucose is from 70 to
110 or only 40 points. Therefore if I overeat my 6:00 AM plan by one silly little slice of
bread my glucose would be 50 points above normal. Obviously I need to be very precise
about insulin doses and food portions.
During the first several years after I was diagnosed I not only regained
the weight I lost during my initial illness but ballooned out to a portly 40 pounds
overweight. Control became difficult at best. I was on a rollercoaster of highs and lows.
At this time I found a doctor that specialized in diabetes and learned more than I had
read in books. My wife and I spent several months working with a dietician. We learned the
principles of diet and changed our eating habits significantly. I lost 55 pounds and
regained control.
Exercise
Exercise is the third traditional element of the balancing plan. Of course
exercise is good for everyone. It makes you feel good, it improves your physical fitness
and generally improves your self-confidence. For the diabetic, exercise lowers blood
glucose and improves insulin sensitivity.
In addition to helping manage current glucose levels exercise is a great
moderator. It sharpens the mind, tones the body, improves heart strength, reduces stress
and fatigue, reduces body fat and improves cholesterol readings. One hour of exercise on a
bicycle has reduced my blood sugar by over 100 points. The benefits of exercise last for
24 hours. Therefore, daily exercise is a must. Anticipation of that exercise in my diet
and insulin levels is also a must.
For me exercise was essential if I were to be with my children as they
grew up. After I learned to manage my insulin and diet I began to ride a bicycle regularly
and developed enough stamina and strength to deal with my children's outings in Boy Scouts
and Girl Scouts. Remember in the early days after insulin was discovered exercise was
often discouraged. I eventually learned how to manage everything and progressed to 90 mile
bicycle rides and weeklong backpacking trips in the Sierras with my sons' Boy Scout Troop.
Other even competed in the Hawaii Ironman competition. Given the lack of clear monitoring
methods exercise seemed to enable me to maintain adequate control.
Self Management
I have often think of diabetes management as driving a car. The gas pedal
makes the car go and the brake pedal stops it. The speedometer tells how fast you are
going. However if you don't watch the speedometer you can get used to speed and soon you
are exceeding the speed limit. How does the diabetic know when he is speeding?
Until the early 1980's the diabetic's speedometer had been awareness of
how they feel. Fatigue and thirstiness indicating high blood sugar or hungry and shaky
indicating low blood sugar. Based on these feelings appropriate action had to be taken.
In the mid-1980's the needed speedometer became widely available. It was a
compact test device that allows an individual to test their blood glucose and get an
answer within one minute. It was a product of evolving blood test techniques, computer
technology and miniaturization techniques.
Test results are obtained from a finger prick of blood. Today's meters not
only test the glucose level but also have added memory and computing capacity to aid the
diabetic in analyzing trends.
Glucose meters allowed the patient to tailor insulin injections to current
glucose levels, the actual time of meals and the content of meals. The techniques that
evolved to integrate diet, exercise, insulin and test results are called flexible
intensive management. Mixed insulin injections which combined the benefits of faster
acting regular insulin with slower acting insulin became more common.
Self testing is now the fourth part of the balancing program to control
diabetes.
The Team
Medical treatment became a team effort intended to guide the patient to
control their diabetes. The team included the patient, the doctor, a certified diabetes
educator (usually a registered nurse or dietician) and a registered dietician. Together
they worked out the techniques that work best for each individual.
What is your number?
Armed with this information, one can knowledgeably adjust insulin,
medication, diet, and exercise regimens to stay in tight control. But what is tight
control?
Interestingly enough at this relatively advanced stage no one had yet
clearly demonstrated in a scientific manner that the underlying assumption of diabetes
management was valid. Again this assumption was that keeping blood glucose close a normal
range would truly extend the diabetics life and maintain good health. With flexible
intensive management and self glucose testing a trial could be designed and conducted.
However how could degree of control be compared?
In the late 1970's a new lab test was developed. This test, the HbA1c or
Glycosylated Hemoglobin test, enabled physicians to determine the time average glucose
level in the patient over the prior two or three months.
The HbA1c blood test measures glycosylated hemoglobin, a molecule in the
blood that allows them to gauge how well they have controlled their blood glucose during
the previous two to three months. Daily blood glucose testing provides only a snapshot of
glycemic control at the moment you test. The HbA1c test gives you the big picture by
showing how you have managed your glucose levels during the previous two to three months. 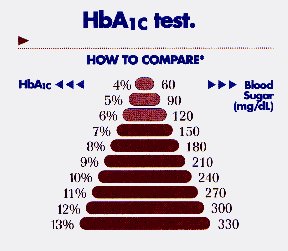
The HbA1c measures the concentration of glycosylated hemoglobin molecules
in the blood. Glycosylated hemoglobin forms when hemoglobin molecules link up with glucose
molecules. The more glucose in the blood, the more hemoglobin becomes glycosylated. Once
glycosylated, hemoglobin stays that way until the red blood cell dies after about 120
days. The HbA1c test can thus determine your average blood glucose level for the previous
two to three months. The result is given as a percentage. Nondiabetics typically have
HbA1c readings of about 4 to 5.5 percent.
A range of 4.4% to 6.4% is considered normal.
Does it all help?
The first comprehensive study to prove the underlying assumption of
diabetes management was sponsored by the National Institute of Diabetes and Digestive and
Kidney Diseases. It proved that keeping blood sugar level as close to normal as safely
possible reduces the risk of developing major complications of diabetes. Many studies have
shown that keeping HbA1c level at 8.1 percent or less helps prevent diabetes related
complications.
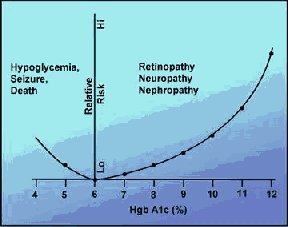 The
10 year study, called the Diabetes Control and Complications Trial, was completed in 1993.
It included 1,441 people with insulin dependant diabetes. The study compared the effect of
two treatment approaches. These were intensive management and standard management on the
development and progression of eye, kidney, and nerve complications of diabetes.
Researchers found that study participants who maintained lower levels of blood glucose
through intensive management had significantly lower rates of these complications.
The
10 year study, called the Diabetes Control and Complications Trial, was completed in 1993.
It included 1,441 people with insulin dependant diabetes. The study compared the effect of
two treatment approaches. These were intensive management and standard management on the
development and progression of eye, kidney, and nerve complications of diabetes.
Researchers found that study participants who maintained lower levels of blood glucose
through intensive management had significantly lower rates of these complications.
Close control of blood glucose levels reduced the risk of eye problems up
to 76%: nerve damage 60% and severe kidney problems 56%.
The Pump
This study also demonstrated the value of another new high tech device
called an insulin pump. An insulin pump is a battery powered computer controlled
electromechanical device about the size of a pack of cigarettes. It contains a reservoir
of insulin connected to tubing and a cannula or needle, which is inserted subcutaneously.
The patient programs the computer to deliver a basal rate of insulin. The patient can give
additional insulin releases called boluses in conjunction with meals or if testing
indicates that blood glucose levels are excessive.
Four years ago I was placed on an insulin pump to improve control of my
glucose levels. I discovered an entirely new level of sophistication in the tools
available to help me. Insulin is delivered continuously. It is delivered as a basal rate
with boluses that I program for meals. In conjunction with the pump is an intensive
testing program requiring a minimum of six blood tests per day. These tests are taken
before each meal and between meals to assure glucose is close to normal.
When my doctor originally suggested an insulin pump I was skeptical. I did
not like the idea of continuous attachment to a box. I read many flowery endorsements that
told how others benefited. I met with the manufacturer's representative but there was no
one to talk to with direct experience. I was the first Inland Empire guinea pig.
It did not take long for me to change my mind. For the first time in 24
years I was no longer under the tyranny of the slow acting insulin shot taken at 6:00 AM
controlling that controlled when I had to eat lunch and dinner. It also allows flexibility
in what can be eaten. If I wanted to eat more I could. Using a pump in conjunction with
fast acting insulin I could quickly bring down high glucose levels. The short acting
insulin combined with regular self-testing also minimizes the possibility of low blood
sugars.
With a pump and a glucose meter you now have a method to know when to step
on the gas or when to step on the brake. You can realistically have a banana split and
still keep your blood glucose close to normal. Or you can safely miss a meal knowing that
you will not experience low blood glucose leading to shakiness or unconsciousness.
In addition with the pump and the tests I have been able to keep my long
term glucose levels below the level at which long term damage occurs.
Almost everyone who uses a pump gains greater blood glucose control. Over
time, improved control significantly reduces your risk of chronic Diabetes complications.
Insulin pumps also help you live a more normal life: You can eat and exercise when you
want and how you want with less fear of experiencing blood glucose ups and downs.
An insulin pump is not an artificial pancreas. It can't measure your blood
glucose level or automatically adjust the amount of insulin you receive. To use a pump,
you must be willing to test your blood glucose at least four to six times a day and learn
how to adjust insulin, diet, and exercise in response to those test results.
More Advances
In recent years, other advances in diabetes research have led to better
ways to manage diabetes and treat its complications.
Other major advances include:
Laser treatment for diabetic eye disease, reducing the risk of blindness
Development of implantable insulin pumps that deliver appropriate
amounts of insulin, replacing daily injections
Successful transplantation of kidneys in people whose own kidneys fail
because of diabetes
Better ways of managing diabetic pregnancies, improving chances of
successful outcomes
New drugs to treat non-insulin dependent diabetes and better ways to
manage this form of diabetes through weight control.
Evidence that intensive management of blood glucose reduces and may
prevent development of microvascular complications of diabetes
Demonstration that antihypertensive drugs called ACE inhibitors prevents
or delays kidney failure in people with diabetes.
The FDA has approved a continuous blood glucose monitor. Currently, it
is limited to use by physicians for patient evaluation. It does offer the future benefit
of warning alarms for patients who are unaware of low blood glucose conditions.
What Will the Future Bring?
In the future, it may be possible to administer insulin through nasal
sprays or in the form of a pill or patch. Devices that can "read" blood glucose
levels without having to prick a finger to get a blood sample are also being developed.
Scientists are looking for genes that may be involved in diabetes. Some
genetic markers have been identified, and it is now possible to screen relatives of people
with diabetes to see if they are at risk.
The new Diabetes Prevention Trial Type I identifies relatives at risk for
developing insulin dependent diabetes and treats them with low doses of insulin or with
oral insulin like agents in the hope of preventing future occurrences.
Transplantation of the pancreas or insulin producing beta cells offers the
best hope of cure for people with insulin dependent diabetes. Some pancreas transplants
have been successful. However, people who have transplants must take powerful drugs to
prevent rejection of the transplanted organ. These drugs are costly and may eventually
cause serious health problems.
Scientists are working to develop less harmful drugs and better methods of
transplanting pancreatic tissue to prevent rejection by the body. Using techniques of
bioengineering, researchers are also trying to create artificial islet cells that secrete
insulin in response to increased sugar levels in the blood.
For non-insulin dependent diabetes, the focus is on ways to prevent
diabetes. Preventive approaches include identifying people at high risk for the disorder
and encouraging them to lose weight, exercise more, and follow a healthy diet.
Bibliography
The National Institute of Diabetes and Digestive and Kidney Diseases of
The National Institutes of Health. Diabetes Overview. Publication No. 96-3873.
October 1995. Last updated: 6 August 1996